"
THIS IS PARKINSON´S
TEN YEARS LATER
"
2014
My arms and legs often shake uncontrollably, and suddenly I can’t move.
If I’m at a café, I sit in the back and order food that’s easy to eat. One time, it took me 45 minutes to get socks on my youngest.
But no one can take away my hope. The hope that one day there will be a miracle cure that lets me function normally again

Arve Sagmo
Share this story
"
2024
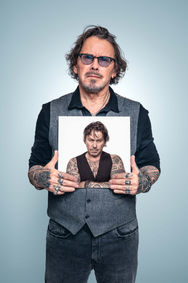
“I actually got pretty sick shortly after we did the photo shoot,” says Arve Sagmo (52). Ten years have passed since I met the airline pilot from Årnes in Romerike, and I think he looks good—but he’s had some tough years.
We’ve just been laughing about what he’s telling me. He’s talking about how mentally exhausting it is to constantly try to hide the symptoms. “It’s not easy to always make sure people don’t notice how I walk, for example.”
It’s been 20 years since he was diagnosed in 2004, at age 32, and still he feels he has to manage everything himself—don’t be a burden, don’t talk about the illness, don’t show symptoms. He doesn’t want people to see that he’s sick. Sometimes that just makes the symptoms worse.
“Have you heard of ‘freezing’? I’m out walking on a deserted road when I see someone coming toward me. Then the stress hits. Now it’s all about not stopping. I keep walking, thinking I’ll make it, but when I’m right next to them, I freeze completely—just stand there, dead still. I can’t move my legs. Honestly, it’s hard. Sometimes I avoid the whole problem by kneeling down well before I meet them and pretending to tie my shoelaces.”
“Do you spend much time with others who have Parkinson’s?”
“No, very little. I played floorball with one guy, but we quit. I’ve been lonely. Got pretty down.”
He has his kids, 12 and 13, every other week. Their mother lives nearby, but they’re divorced now. And he has two older kids from a previous relationship who live farther away.
“I see a psychologist now, and I’m in group therapy. Parkinson’s is something you almost have to experience to understand. Physically, it’s like every muscle in your body is in full tension.”
Arve has DBS (Deep Brain Stimulation) with electrodes implanted in his brain and takes much less Parkinson’s medication than before—just 4x50 mg Sinemet, plus Remeron and Cipralex for his mental health. At one point, he was taking meds ten times a day: 1250 mg Stalevo, 8 mg Requip, plus Azilect—and still felt worse than he does now. When he arrived at Rikshospitalet for surgery, he could barely walk to the entrance. DBS was his lifeline.
“After the DBS surgery in 2016, I felt great—but after a few weeks, I noticed something was wrong. They’d told me to watch closely because an infection could be very serious, so when I saw swelling on my chest over the stimulator, I went to Rikshospitalet. I had an infection throughout the system. Everything had to come out, and I had to go without it for a couple of months. Even the electrodes had to be removed. It was awful—it could have gone really badly.”
“In 2017, they did the whole procedure again. Since then, it’s worked well. The device has only been adjusted once. Without DBS, my life would be very different.”
Arve is still working. He does administrative tasks at a metal industry company. He has wage subsidies from NAV and works 50%.
His symptoms are rigidity, stiffness, some dyskinesia, and a shuffling gait. He’s never been on a rehab stay. He was offered a spot once but declined because of illness in the family. He doesn’t have an assistant like some others do. He hasn’t experienced personality changes. He feels things are a bit better now and has reconnected with some friends. He’s happy to share his story if it can help someone.
“When I got the diagnosis, I was only 32 and didn’t know there were other young people with Parkinson’s. And a lot has improved. Now I know there are medications and surgeries that make it possible to function for many years, and that the disease isn’t a death sentence like I thought back then. And I still have hope for a cure—but I understand now that research takes time.”